Cytokines Activate T Helper Cells
A second role of helper T cells is to help B cells respond to antigens. Many antigens cannot by themselves cause a specific B cell to divide into a clone of.
Helper T cells are arguably the most important cells in adaptive immunity, as they are required for almost all adaptive immune responses. They not only help activate.

In 1986, Mosmann and Coffman introduced the concept of distinct types of helper T cells, which was based on the types of cytokines that T cells produce when they are.

Apr 02, 2015 Characterization of Follicular Helper T Cells Dylan Djani December 4th, 2012 MICRO H414 Basic Immunology Dr. Charlie Wei.
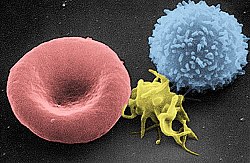
Scanning electron micrograph of a human T cell
T cells or T lymphocytes are a type of lymphocyte in turn, a type of white blood cell that play a central role in cell-mediated immunity. They can be distinguished from other lymphocytes, such as B cells and natural killer cells NK cells, by the presence of a T-cell receptor TCR on the cell surface. They are called T cells because they mature in the thymus 1 although some also mature in the tonsils 2. The several subsets of T cells each have a distinct function. The majority of human T cells rearrange their alpha/beta T cell receptors and are termed alpha beta T cells and are part of adaptive immune system. Specialized gamma delta T cells, which comprise a minority of T cells in the human body more frequent in ruminants, have invariant TCR with limited diversity, can effectively present antigens to other T cells 3 and are considered to be part of the innate immune system.
1.6 Mucosal associated invariant
T helper cells TH cells assist other white blood cells in immunologic processes, including maturation of B cells into plasma cells and memory B cells, and activation of cytotoxic T cells and macrophages. These cells are also known as CD4 T cells because they express the CD4 glycoprotein on their surfaces. Helper T cells become activated when they are presented with peptide antigens by MHC class II molecules, which are expressed on the surface of antigen-presenting cells APCs. Once activated, they divide rapidly and secrete small proteins called cytokines that regulate or assist in the active immune response. These cells can differentiate into one of several subtypes, including TH1, TH2, TH3, TH17, Th9, or TFH, which secrete different cytokines to facilitate different types of immune responses. Signalling from the APC directs T cells into particular subtypes. 4
Cytotoxic T cells TC cells, or CTLs destroy virus-infected cells and tumor cells, and are also implicated in transplant rejection. These cells are also known as CD8 T cells since they express the CD8 glycoprotein at their surfaces. These cells recognize their targets by binding to antigen associated with MHC class I molecules, which are present on the surface of all nucleated cells. Through IL-10, adenosine, and other molecules secreted by regulatory T cells, the CD8 cells can be inactivated to an anergic state, which prevents autoimmune diseases.
Memory T cells are a subset of antigen-specific T cells that persist long-term after an infection has resolved. They quickly expand to large numbers of effector T cells upon re-exposure to their cognate antigen, thus providing the immune system with memory against past infections. Memory T cells comprise three subtypes: central memory T cells TCM cells, effector memory T cells TEM cells and TEMRA cells 5 and resident memory T cells TRM. 6 Memory cells may be either CD4 or CD8. Memory T cells typically express the cell surface protein CD45RO. 7
Suppressor T cells are crucial for the maintenance of immunological tolerance. Their major role is to shut down T cell-mediated immunity toward the end of an immune reaction and to suppress autoreactive T cells that escaped the process of negative selection in the thymus. Suppressor T cells along with Helper T cells can collectively be called Regulatory T cells due to their regulatory functions. 8
Two major classes of CD4 Treg cells have been described FOXP3 Treg cells and FOXP3 Treg cells.
Regulatory T cells can develop either during normal development in the thymus, and are then known as thymic Treg cells, or can be induced peripherally and are called peripherally derived Treg cells. These two subsets were previously called naturally occurring, and adaptive or induced, respectively. 9 Both subsets require the expression of the transcription factor FOXP3 which can be used to identify the cells. Mutations of the FOXP3 gene can prevent regulatory T cell development, causing the fatal autoimmune disease IPEX.
Several other types of T cell have suppressive activity, but do not express FOXP3. These include Tr1 cells and Th3 cells, which are thought to originate during an immune response and act by producing suppressive molecules. Tr1 cells are associated with IL-10, and Th3 cells are associated with TGF-beta. Recently, Treg17 cells have been added to this list. 10
Natural killer T cells NKT cells – not to be confused with natural killer cells of the innate immune system bridge the adaptive immune system with the innate immune system. Unlike conventional T cells that recognize peptide antigens presented by major histocompatibility complex MHC molecules, NKT cells recognize glycolipid antigen presented by a molecule called CD1d. Once activated, these cells can perform functions ascribed to both Th and Tc cells i.e., cytokine production and release of cytolytic/cell killing molecules. They are also able to recognize and eliminate some tumor cells and cells infected with herpes viruses. citation needed
Mucosal associated invariant edit
Mucosal associated invariant T cells are a special type of T cell. citation needed
Gamma delta T cells γδ T cells represent a small subset of T cells that possess a distinct T cell receptor TCR on their surfaces. A majority of T cells have a TCR composed of two glycoprotein chains called α- and β- TCR chains. However, in γδ T cells, the TCR is made up of one γ-chain and one δ-chain. This group of T cells is much less common in humans and mice about 2 of total T cells ; and are found in the highest abundance in the gut mucosa, within a population of lymphocytes known as intraepithelial lymphocytes. In rabbits, sheep, and chickens, the number of γδ T cells can be as high as 60 of total T cells. The antigenic molecules that activate γδ T cells are still widely unknown. However, γδ T cells are not MHC-restricted and seem to be able to recognize whole proteins rather than requiring peptides to be presented by MHC molecules on APCs. Some murine γδ T cells recognize MHC class IB molecules, though. Human Vγ9/Vδ2 T cells, which constitute the major γδ T cell population in peripheral blood, are unique in that they specifically and rapidly respond to a set of nonpeptidic phosphorylated isoprenoid precursors, collectively named phosphoantigens, which are produced by virtually all living cells. The most common phosphoantigens from animal and human cells including cancer cells are isopentenyl pyrophosphate IPP and its isomer dimethylallyl pyrophosphate DMPP. Many microbes produce the highly active compound hydroxy-DMAPP HMB-PP and corresponding mononucleotide conjugates, in addition to IPP and DMAPP. Plant cells produce both types of phosphoantigens. Drugs activating human Vγ9/Vδ2 T cells comprise synthetic phosphoantigens and aminobisphosphonates, which upregulate endogenous IPP/DMAPP.
Development in the thymus edit
All T cells originate from haematopoietic stem cells in the bone marrow. Haematopoietic progenitors lymphoid progenitor cells from haematopoietic stem cells populate the thymus and expand by cell division to generate a large population of immature thymocytes. 11 The earliest thymocytes express neither CD4 nor CD8, and are therefore classed as double-negative CD4 CD8 cells. As they progress through their development, they become double-positive thymocytes CD4 CD8, and finally mature to single-positive CD4 CD8 or CD4 CD8 thymocytes that are then released from the thymus to peripheral tissues.
About 98 of thymocytes die during the development processes in the thymus by failing either positive selection or negative selection, whereas the other 2 survive and leave the thymus to become mature immunocompetent T cells. Increasing evidence indicates microRNAs, which are small noncoding regulatory RNAs, could impact the clonal selection process during thymic development. For example, miR-181a was found to play a role in the positive selection of T lymphocytes. 12
The thymus contributes fewer cells as a person ages. As the thymus shrinks by about 3 13 a year throughout middle age, a corresponding fall in the thymic production of naive T cells occurs, leaving peripheral T cell expansion to play a greater role in protecting older subjects.
Common lymphoid precursor cells that migrate to the thymus become known as T-cell precursors or thymocytes and do not express a T cell receptor. Broadly speaking, the double negative DN stage is focused on producing a functional β-chain whereas the double positive DP stage is focused on producing a functional α-chain, ultimately producing a functional αβ T cell receptor. As the developing thymocyte progresses through the four DN stages DN1, DN2, DN3, and DN4, the T cell expresses an invariant α-chain but rearranges the β-chain locus. If the rearranged β-chain successfully pairs with the invariant α-chain, signals are produced which cease rearrangement of the β-chain and silence the alternate allele and result in proliferation of the cell. 14 Although these signals require this pre-TCR at the cell surface, they are independent of ligand binding to the pre-TCR. These thymocytes will then express both CD4 and CD8 and progresses to the double positive DP stage where selection of the α-chain takes place. If a rearranged β-chain does not lead to any signalling e.g. as a result of an inability to pair with the invariant α-chain, the cell may die by neglect lack of signalling.
Positive selection selects for T cells capable of interacting with MHC. Double-positive thymocytes CD4 /CD8 move deep into the thymic cortex, where they are presented with self-antigens. These self-antigens are expressed by thymic cortical epithelial cells on MHC molecules on the surface of cortical epithelial cells. Only those thymocytes that interact with MHC-I or MHC-II appropriately i.e., not too strongly or too weakly will receive a vital survival signal. All that cannot i.e., if they do not interact strongly enough, or if they bind too strongly will die by death by neglect no survival signal. This process ensures that the selected T-cells will have an MHC affinity that can serve useful functions in the body i.e., the cells must be able to interact with MHC and peptide complexes to effect immune responses. The vast majority of all thymocytes end up dying during this process.
A thymocyte s fate is determined during positive selection. Double-positive cells CD4 /CD8 that interact well with MHC class II molecules will eventually become CD4 cells, whereas thymocytes that interact well with MHC class I molecules mature into CD8 cells. A T cell becomes a CD4 cell by down-regulating expression of its CD8 cell surface receptors. If the cell does not lose its signal, it will continue downregulating CD8 and become a CD4, single positive cell. But, if there is a signal interruption, the cell stops downregulating CD8 and switches over to downregulating CD4 molecules, instead, eventually becoming a CD8, single positive cell.
This process does not remove thymocytes that may cause autoimmunity. The potentially autoimmune cells are removed by the process of negative selection, which occurs in the thymic medulla discussed below.
Negative selection removes thymocytes that are capable of strongly binding with self MHC peptides. Thymocytes that survive positive selection migrate towards the boundary of the cortex and medulla in the thymus. While in the medulla, they are again presented with a self-antigen presented on the MHC complex of medullary thymic epithelial cells mTECs. 15 mTECs must be AIRE to properly express self-antigens from all tissues of the body on their MHC class I peptides. Some mTECs are phagocytosed by thymic dendritic cells; this allows for presentation of self-antigens on MHC class II molecules positively selected CD4 cells must interact with MHC class II molecules, thus APCs, which possess MHC class II, must be present for CD4 T-cell negative selection. Thymocytes that interact too strongly with the self-antigen receive an apoptotic signal that leads to cell death. However, some of these cells are selected to become Treg cells. The remaining cells exit the thymus as mature naive T cells also known as recent thymic emigrants. This process is an important component of central tolerance and serves to prevent the formation of self-reactive T cells that are capable of inducing autoimmune diseases in the host.
In summary, β-selection is the first checkpoint, where the T cells that are able to form a functional pre-TCR with an invariant alpha chain and a functional beta chain are allowed to continue development in the thymus. Next, positive selection checks that T cells have successfully rearranged their TCRα locus and are capable of recognizing peptide-MHC complexes with appropriate affinity. Negative selection in the medulla then obliterates T cells that bind too strongly to self-antigens expressed on MHC molecules. These selection processes allow for tolerance of self by the immune system. Typical T-cells that leave the thymus via the corticomedullarly junction are self-restricted, self-tolerant, and singly positive.
The T lymphocyte activation pathway: T cells contribute to immune defenses in two major ways; some direct and regulate immune responses; others directly attack infected or cancerous cells. 16
Activation of CD4 T cells occurs through the simultaneous engagement of the T cell receptor and a costimulatory molecule like CD28, or ICOS on the T cell by the major histocompatibility complex MHCII peptide and costimulatory molecules on the APC. Both are required for production of an effective immune response; in the absence of costimulation, T-cell receptor signalling alone results in anergy. The signalling pathways downstream from costimulatory molecules usually engages the PI3K pathway generating PIP3 at the plasma membrane and recruiting PH domain containing signaling molecules like PDK1 that are essential for the activation of PKCθ, and eventual IL-2 production.
The first signal is provided by binding of the T cell receptor to its cognate peptide presented on MHCII on an APC. MHCII is restricted to so-called professional APCs, like dendritic cells, B cells, and macrophages, to name a few. The peptides presented to CD8 T cells by MHC class I molecules are 8–9 amino acids in length; the peptides presented to CD4 cells by MHC class II molecules are longer, usually 12–25 amino acids in length, 17 as the ends of the binding cleft of the MHC class II molecule are open.
The second signal comes from costimulation, in which surface receptors on the APC are induced by a relatively small number of stimuli, usually products of pathogens, but sometimes breakdown products of cells, such as necrotic-bodies or heat shock proteins. The only costimulatory receptor expressed constitutively by naïve T cells is CD28, so costimulation for these cells comes from the CD80 and CD86 proteins, which together constitute the B7 protein, B7.1 and B7.2, respectively on the APC. Other receptors are expressed upon activation of the T cell, such as OX40 and ICOS, but these largely depend upon CD28 for their expression. The second signal licenses the T cell to respond to an antigen. Without it, the T cell becomes anergic, and it becomes more difficult for it to activate in future. This mechanism prevents inappropriate responses to self, as self-peptides will not usually be presented with suitable costimulation. Once a T cell has been appropriately activated i.e. has received signal one and signal two it alters its cell surface expression of a variety of proteins. Markers of T cell activation include CD69, CD71 and CD25 also a marker for Treg cells, and HLA-DR a marker of human T cell activation. CTLA-4 expression is also up-regulated on activated T cells, which in turn outcompetes CD28 for binding to the B7 proteins. This is a checkpoint mechanism to prevent over activation of the T cell. Activated T cells also change their cell surface glycosylation profile. 18
The T cell receptor exists as a complex of several proteins. The actual T cell receptor is composed of two separate peptide chains, which are produced from the independent T cell receptor alpha and beta TCRα and TCRβ genes. The other proteins in the complex are the CD3 proteins: CD3εγ and CD3εδ heterodimers and, most important, a CD3ζ homodimer, which has a total of six ITAM motifs. The ITAM motifs on the CD3ζ can be phosphorylated by Lck and in turn recruit ZAP-70. Lck and/or ZAP-70 can also phosphorylate the tyrosines on many other molecules, not least CD28, LAT and SLP-76, which allows the aggregation of signalling complexes around these proteins.
Phosphorylated LAT recruits SLP-76 to the membrane, where it can then bring in PLC-γ, VAV1, Itk and potentially PI3K. PLC-γ cleaves PI 4,5 P2 on the inner leaflet of the membrane to create the active intermediaries diacylglycerol DAG, inositol-1,4,5-trisphosphate IP3 ; PI3K also acts on PIP2, phosphorylating it to produce phosphatidlyinositol-3,4,5-trisphosphate PIP3. DAG binds and activates some PKCs. Most important in T cells is PKCθ, critical for activating the transcription factors NF-κB and AP-1. IP3 is released from the membrane by PLC-γ and diffuses rapidly to activate calcium channel receptors on the ER, which induces the release of calcium into the cytosol. Low calcium in the endoplasmic reticulum causes STIM1 clustering on the ER membrane and leads to activation of cell membrane CRAC channels that allows additional calcium to flow into the cytosol from the extracellular space. This aggregated cytosolic calcium binds calmodulin, which can then activate calcineurin. Calcineurin, in turn, activates NFAT, which then translocates to the nucleus. NFAT is a transcription factor that activates the transcription of a pleiotropic set of genes, most notable, IL-2, a cytokine that promotes long-term proliferation of activated T cells.
PLCγ can also initiate the NF-κB pathway. DAG activates PKCθ, which then phosphorylates CARMA1, causing it to unfold and function as a scaffold. The cytosolic domains bind an adapter BCL10 via CARD Caspase activation and recruitment domains domains; that then binds TRAF6, which is ubiquitinated at K63.Template:Rp:513–523 19 This form of ubiquitination does not lead to degradation of target proteins. Rather, it serves to recruit NEMO, IKKα and -β, and TAB1-2/ TAK1. 20 TAK 1 phosphorylates IKK-β, which then phosphorylates IκB allowing for K48 ubiquitination: leads to proteosomal degradation. Rel A and p50 can then enter the nucleus and bind the NF-κB response element. This coupled with NFAT signaling allows for complete activation of the IL-2 gene. 19
While in most cases activation is dependent on TCR recognition of antigen, alternative pathways for activation have been described. For example, cytotoxic T cells have been shown to become activated when targeted by other CD8 T cells leading to tolerization of the latter. 21
In spring 2014, the T-Cell Activation in Space TCAS experiment was launched to the International Space Station on the SpaceX CRS-3 mission to study how deficiencies in the human immune system are affected by a microgravity environment 22
A unique feature of T cells is their ability to discriminate between healthy and abnormal e.g. infected or cancerous cells in the body. 23 Healthy cells typically express a large number of self derived pMHC on their cell surface and although the T cell antigen receptor can interact with at least a subset of these self pMHC, the T cell generally ignores these healthy cells. However, when these very same cells contain even minute quantities of pathogen derived pMHC, T cells are able to become activated and initiate immune responses. The ability of T cells to ignore healthy cells but respond when these same cells contain pathogen or cancer derived pMHC is known as antigen discrimination. The molecular mechanisms that underlie this process are controversial. 23 24
In 2015, a team of researchers led by Dr. Alexander Marson 25 at the University of California, San Francisco successfully edited the genome of human T cells using a Cas9 ribonucleoprotein delivery method. 26 This advancement has potential for applications in treating cancer immunotherapies and cell-based therapies for HIV, primary immune deficiencies, and autoimmune diseases. 26
Main article: T cell deficiency
Causes of T cell deficiency include lymphocytopenia of T cells and/or defects on function of individual T cells. Complete insufficiency of T cell function can result from hereditary conditions such as severe combined immunodeficiency SCID, Omenn syndrome, and Cartilage-hair hypoplasia. 27 Causes of partial insufficiencies of T cell function include acquired immune deficiency syndrome AIDS, and hereditary conditions such as DiGeorge syndrome DGS, chromosomal breakage syndromes CBSs, and B-cell and T-cell combined disorders such as ataxia telangiectasia AT and Wiskott-Aldrich syndrome WAS. 27
The main pathogens of concern in T cell deficiencies are intracellular pathogens, including Herpes simplex virus, Mycobacterium and Listeria. 28 Also, fungal infections are also more common and severe in T cell deficiencies. 28
Further information: T-cell lymphoma
Cancer of T cells is termed T-cell lymphoma, and accounts for perhaps one in ten cases of non-Hodgkin lymphoma. 29 The main forms of T cell lymphoma are:
Cutaneous T cell lymphomas: Sézary syndrome and Mycosis fungoides
Anaplastic large cell lymphoma
Angioimmunoblastic T cell lymphoma
T-cell exhaustion is the progressive loss of T-cell function. It can occur during sepsis and after other acute or chronic infections. 30 31
Alberts B, Johnson A, Lewis J, Raff M, Roberts k, Walter P 2002 Molecular Biology of the Cell. Garland Science: New York, NY pg 1367. T cells and B cells derive their names from the organs in which they develop. T cells develop in the thymus, and B cells, in mammals, develop in the bone marrow in adults or the liver in fetuses.
McClory, Susan; Hughes, Tiffany; Freud, Aharon G.; Briercheck, Edward L.; Martin, Chelsea; Trimboli, Anthony J.; Yu, Jianhua; Zhang, Xiaoli; Leone, Gustavo Apr 2012. Evidence for a stepwise program of extrathymic T cell development within the human tonsil. The Journal of Clinical Investigation 122 4 : 1403–1415. doi:10.1172/JCI46125. ISSN 1558-8238. PMC 3314444. PMID 22378041.
Vantourout, Pierre; Hayday, Adrian Feb 2013. Six-of-the-best: unique contributions of γδ T cells to immunology. Nature Reviews. Immunology 13 2 : 88–100. doi:10.1038/nri3384. ISSN 1474-1741. PMC 3951794. PMID 23348415.
Gutcher I, Becher B 2007. APC-derived cytokines and T cell polarization in autoimmune inflammation. J. Clin. Invest. 117 5 : 1119–27. doi:10.1172/JCI31720. PMC 1857272. PMID 17476341.
Willinger T, Freeman T, Hasegawa H, McMichael AJ, Callan MF 2005. Molecular signatures distinguish human central memory from effector memory CD8 T cell subsets.. Journal of Immunology 175 9 : 5895–903. doi:10.4049/jimmunol.175.9.5895. PMID 16237082.
Shin, Haina; Iwasaki, Akiko 2013-09-01. Tissue-resident memory T cells. Immunological Reviews 255 1 : 165–181. doi:10.1111/imr.12087. ISSN 1600-065X. PMC 3748618. PMID 23947354.
Akbar AN, Terry L, Timms A, Beverley PC, Janossy G April 1988. Loss of CD45R and gain of UCHL1 reactivity is a feature of primed T cells. J. Immunol. 140 7 : 2171–8. PMID 2965180.
Textbook of Medical Physiology by Guyton and Hall, edition 6, pg. 448, Suppressor T cells paragraph.
Abbas AK, Benoist C, Bluestone JA, Campbell DJ, Ghosh S, Hori S, Jiang S, Kuchroo VK, Mathis D, Roncarolo MG, Rudensky A, Sakaguchi S, Shevach EM, Vignali DA, Ziegler SF 2013. Regulatory T cells: recommendations to simplify the nomenclature. Nat. Immunol. 14 4 : 307–8. doi:10.1038/ni.2554. PMID 23507634.
Singh B, Schwartz JA, Sandrock C, Bellemore SM, Nikoopour E 2013. Modulation of autoimmune diseases by interleukin IL -17 producing regulatory T helper Th17 cells. Indian J. Med. Res. 138 5 : 591–4. PMC 3928692. PMID 24434314.
Schwarz BA, Bhandoola A February 2006. Trafficking from the bone marrow to the thymus: a prerequisite for thymopoiesis. Immunol. Rev. 209: 47–57. doi:10.1111/j.0105-2896.2006.00350.x. PMID 16448533.
Li QJ, Chau J, Ebert PJ, Sylvester G, Min H, Liu G, Braich R, Manoharan M, Soutschek J, Skare P, Klein LO, Davis MM, Chen CZ 2007. miR-181a is an intrinsic modulator of T cell sensitivity and selection. Cell 129 1 : 147–61. doi:10.1016/j.cell.2007.03.008. PMID 17382377.
Haynes BF, Markert ML, Sempowski GD, Patel DD, Hale LP 2000. The role of the thymus in immune reconstitution in aging, bone marrow transplantation, and HIV-1 infection. Annu. Rev. Immunol. 18: 529–60. doi:10.1146/annurev.immunol.18.1.529. PMID 10837068.
Janeway, Charles 2012. Immunobiology. Garland Science. pp. 301–305. ISBN 9780815342434.
Hinterberger M, Aichinger M, Prazeres da Costa O, Voehringer D, Hoffmann R, Klein L June 2010. Autonomous role of medullary thymic epithelial cells in central CD4 T cell tolerance. Nat. Immunol. 11 6 : 512–9. doi:10.1038/ni.1874. PMID 20431619.
The NIAID resource booklet Understanding the Immune System pdf.
Jennifer Rolland and Robyn O Hehir, Turning off the T-cells: Peptides for treatment of allergic Diseases, Today s life science publishing, 1999, Page 32
Maverakis E, Kim K, Shimoda M, Gershwin M, Patel F, Wilken R, Raychaudhuri S, Ruhaak LR, Lebrilla CB 2015. Glycans in the immune system and The Altered Glycan Theory of Autoimmunity. J Autoimmun 57 6 : 1–13. doi:10.1016/j.jaut.2014.12.002. PMID 25578468.
a b Tatham P, Gomperts BD, Kramer IM 2003. Signal transduction. Amsterdam: Elsevier Academic Press. ISBN 0-12-289632-7.
Wu H, Arron JR November 2003. TRAF6, a molecular bridge spanning adaptive immunity, innate immunity and osteoimmunology. BioEssays 25 11 : 1096–105. doi:10.1002/bies.10352. PMID 14579250.
Milstein O, Hagin D, Lask A, Reich-Zeliger S, Shezen E, Ophir E, Eidelstein Y, Afik R, Antebi YE, Dustin ML, Reisner Y January 2011. CTLs respond with activation and granule secretion when serving as targets for T-cell recognition. Blood 117 3 : 1042–52. doi:10.1182/blood-2010-05-283770. PMC 3035066. PMID 21045195.
Graham, William 2014-04-14. SpaceX ready for CRS-3 Dragon launch and new milestones. NASAspaceflight.com. Retrieved 2014-04-14.
a b Feinerman O, Germain RN, Altan-Bonnet G 2008. Quantitative challenges in understanding ligand discrimination by alphabeta T cells. Mol. Immunol. 45 3 : 619–31. doi:10.1016/j.molimm.2007.03.028. PMC 2131735. PMID 17825415.
Dushek O, van der Merwe PA 2014. An induced rebinding model of antigen discrimination. Trends Immunol. 35 4 : 153–8. doi:10.1016/j.it.2014.02.002. PMC 3989030. PMID 24636916.
a b Schumann, Kathrin; Lin, Steven; Boyer, Eric; Simeonov, Dimitre R.; Subramaniam, Meena; Gate, Rachel E.; Haliburton, Genevieve E.; Ye, Chun J.; Bluestone, Jeffrey A. 2015-08-18. Generation of knock-in primary human T cells using Cas9 ribonucleoproteins. Proceedings of the National Academy of Sciences of the United States of America 112 33 : 10437–10442. doi:10.1073/pnas.1512503112. ISSN 1091-6490. PMC 4547290. PMID 26216948.
a b Medscape T-cell Disorders. Author: Robert A Schwartz, MD, MPH; Chief Editor: Harumi Jyonouchi, MD. Updated: May 16, 2011
a b Jones J, Bannister BA, Gillespie SH, ed. 2006. Infection: Microbiology and Management. Wiley-Blackwell. p. 435. ISBN 1-4051-2665-5.
The Lymphomas PDF. The Leukemia Lymphoma Society. May 2006. p. 2. Retrieved 2008-04-07.
John S Yi, Maureen A Cox, and Allan J Zajac Apr 2010. T-cell exhaustion: characteristics, causes and conversion. Immunology 129 4 : 474–481. doi:10.1111/j.1365-2567.2010.03255.x. PMC 2842494.
Hotchkiss RS, Monneret G, Payen D. Mar 2013. Immunosuppression in sepsis: a novel understanding of the disorder and a new therapeutic approach. Lancet Infect Dis 13 3 : 260–8. doi:10.1016/S1473-3099 13 70001-X.
niaid.nih.gov – The Immune System
T-cell Group – Cardiff University
Successful. Treatment of Metastatic Melanoma with Autologous CD4 T Cells against NY-ESO-1.
The Center for Modeling Immunity to Enteric Pathogens MIEP
Davies AJ 1993. The tale of T cells. Immunology Today 14 3 : 137–139. doi:10.1016/0167-5699 93 90216-8. PMID 8466629.
Retrieved from https://en.wikipedia.org/w/index.php.title T_cell oldid 690133445
Categories: T cellsHuman cellsImmune systemImmunology.

Proposed effector activities of T helper 9 T H 9 cells in human disease are shown. a The number of T H 9 cells present in the draining lymph nodes and the airways.
Activation of naïve helper T cells. Following T cell development, matured, naïve T cells leave the thymus and begin to spread throughout the body, including the.
The T helper cells Th cells are a type of T cell that play an important role in the immune system, particularly in the adaptive immune system. They help the activity of other immune cells by releasing T cell cytokines. These cells help suppress or regulate immune responses. They are essential in B cell antibody class switching, in the activation and growth of cytotoxic T cells, and in maximizing bactericidal activity of phagocytes such as macrophages.
Mature Th cells express the surface protein CD4 and are referred to as CD4 T cells. Such CD4 T cells are generally treated as having a pre-defined role as helper T cells within the immune system. For example, when an antigen-presenting cell expresses an antigen on MHC class II, a CD4 cell will aid those cells through a combination of cell to cell interactions e.g. CD40 and CD40L and through cytokines. Nevertheless, there are rare exceptions; for example, sub-groups of regulatory T cells, natural killer cells, and cytotoxic T cells express CD4. All of the latter CD4 T cell groups are not considered T helper cells.
The importance of helper T cells can be seen from HIV, a virus that primarily infects CD4 T cells. In the advanced stages of HIV infection, loss of functional CD4 T cells leads to the symptomatic stage of infection known as the acquired immunodeficiency syndrome AIDS. When the HIV virus is detected early in blood or other bodily fluids, continuous therapy can delay the time at which this fall happens. Therapy can also better manage the course of AIDS if and when it occurs. There are other rare disorders such as lymphocytopenia which result in the absence or dysfunction of CD4 T cells. These disorders produce similar symptoms, many of which are fatal.
1 Activation of naïve helper T cells
2 Determination of the effector T cell response
2.1 Th1/Th2 Model for helper T cells
2.4 Limitations to the Th1/Th2 model
3 Role of helper T cells in disease
3.2 Helper T cells and hypersensitivity
Activation of naïve helper T cells edit
Following T cell development, matured, naïve T cells leave the thymus and begin to spread throughout the body, including the lymph nodes. Naïve T cells are those T cells that have never been exposed to the antigen that they are programmed to respond to. Like all T cells, they express the T cell receptor-CD3 complex. The T cell receptor TCR consists of both constant and variable regions. The variable region determines what antigen the T cell can respond to. CD4 T cells have TCRs with an affinity for Class II MHC, and CD4 is involved in determining MHC affinity during maturation in the thymus. Class II MHC proteins are generally only found on the surface of specialised antigen-presenting cells APCs. Specialised antigen presenting cells are primarily dendritic cells, macrophages and B cells, although dendritic cells are the only cell group that expresses MHC Class II constitutively at all times. Some APCs also bind native or unprocessed antigens to their surface, such as follicular dendritic cells, but unprocessed antigens do not interact with T cells and are not involved in their activation. The antigens that bind to MHC proteins are always short peptides, 8-10 amino acids long for MHC Class I, and up to 25 or so for MHC Class II.
Antigen presentation stimulates T cells to become either cytotoxic CD8 cells or helper CD4 cells.
During an immune response, professional antigen-presenting cells APCs endocytose foreign material typically bacteria or viruses, which undergoes processing, then travel from the infection site to the lymph nodes. Once at the lymph nodes, the APC begin to present antigen peptides that are bound to Class II MHC, allowing CD4 T cells that express the specific TCRs against the peptide/MHC complex to activate.
When a Th cell encounters and recognises the antigen on an APC, the TCR-CD3 complex binds strongly to the peptide-MHC complex present on the surface of professional APCs. CD4, a co-receptor of the TCR complex, also binds to a different section of the MHC molecule. These interactions bring these proteins closer together, allowing the intracellular kinases present on the TCR, CD3 and CD4 proteins to activate each other via phosphorylation. With the assistance of a phosphatase present on the intracellular section of CD45 common leukocyte antigen, these molecules activate major Th cell intracellular pathways. These active pathways are known as Signal 1 of T cell activation, as it is the first and primary pro-activation signal in a Th cell. Upon subsequent encounters with a given antigen, memory T cells are re-activated using the same TCR pathways.
The binding of the antigen-MHC to the TCR complex and CD4 may also help the APC and the Th cell adhere during Th cell activation, but the integrin protein LFA-1 on the T cell and ICAM on the APC are the primary molecules of adhesion in this cell interaction.
It is unknown what role the relatively bulky extracellular region of CD45 plays during cell interactions, but CD45 has various isoforms that change in size depending on the Th cell s activation and maturation status. For example, CD45 shortens in length following Th activation CD45RA to CD45RO, but whether this change in length influences activation is unknown. It has been proposed that the larger CD45RA may decrease the accessibility of the T cell receptor for the antigen-MHC molecule, thereby necessitating an increase in the affinity and specificity of the T cell for activation. Once the activation has occurred however, CD45 shortens, allowing easier interactions and activation as an effector T helper cell. citation needed
Having received the first TCR/CD3 signal, the naïve T cell must activate a second independent biochemical pathway, known as Signal 2. This verification step is a protective measure to ensure that a T cell is responding to a foreign antigen. If this second signal is not present during initial antigen exposure, the T cell presumes that it is auto-reactive. This results in the cell becoming anergic anergy is generated from the unprotected biochemical changes of Signal 1. Anergic cells will not respond to any antigen in the future, even if both signals are present later on. These cells are generally believed to circulate throughout the body with no value until they undergo apoptosis.
The second signal involves an interaction between CD28 on the CD4 T cell and the proteins CD80 B7.1 or CD86 B7.2 on the professional APCs. Both CD80 and CD86 activate the CD28 receptor. These proteins are also known as co-stimulatory molecules.
Although the verification stage is necessary for the activation of naïve helper T cells, the importance of this stage is best demonstrated during the similar activation mechanism of CD8 cytotoxic T cells. As naïve CD8 T cells have no true bias towards foreign sources, these T cells must rely on the activation of CD28 for confirmation that they recognise a foreign antigen as CD80/CD86 is only expressed by active APC s. CD28 plays an important role in decreasing the risk of T cell auto-immunity against host antigens.
Once the naïve T cell has both pathways activated, the biochemical changes induced by Signal 1 are altered, allowing the cell to activate instead of anergise. The second signal is then obsolete; only the first signal is necessary for future activation. This is also true for memory T cells, which is one example of learned immunity. Faster responses occur upon reinfection because memory T cells have already undergone confirmation and can produce effector cells much sooner.
Once the two-signal activation is complete the T helper cell Th then allows itself to proliferate. It achieves this by releasing a potent T cell growth factor called interleukin 2 IL-2 which acts upon itself in an autocrine fashion. Activated T cells also produce the alpha sub-unit of the IL-2 receptor CD25 or IL-2R, enabling a fully functional receptor that can bind with IL-2, which in turn activates the T cell s proliferation pathways.
The autocrine or paracrine secretion of IL-2 can bind that same Th cell or neighboring Th s via the IL-2R thus driving proliferation and clonal expansion. The Th cells receiving both signals of activation and proliferation will then become Th0 cells T helper 0 cell that secrete IL-2, IL-4 and interferon gamma IFN-γ. The Th0 cells will then differentiate into Th1 or Th2 cells depending on cytokine environment. IFN-γ drives Th1 cell production while IL-10 and IL-4 inhibit Th1 cell production. Conversely, IL-4 drives Th2 cell production and IFN-γ inhibits Th2 cells. It should be noted that these cytokines are pleiotropic and carry out many other functions of the immune response.
After many cell generations, the Th cell s progenitors differentiate into effector Th cells, memory Th cells, and regulatory Th cells.
Effector Th cells secrete cytokines, proteins or peptides that stimulate or interact with other leukocytes, including Th cells.
Memory Th cells retain the antigen affinity of the originally activated T cell, and are used to act as later effector cells during a second immune response e.g. if there is re-infection of the host at a later stage.
Regulatory T cells do not promote immune function, but act to decrease it instead. Despite their low numbers during an infection, these cells are believed to play an important role in the self-limitation of the immune system; they have been shown to prevent the development of various autoimmune diseases.
Determination of the effector T cell response edit
Helper T cells are capable of influencing a variety of immune cells, and the T cell response generated including the extracellular signals such as cytokines can be essential for a successful outcome from infection. In order to be effective, helper T cells must determine which cytokines will allow the immune system to be most useful or beneficial for the host. Understanding exactly how helper T cells respond to immune challenges is currently of major interest in immunology, because such knowledge may be very useful in the treatment of disease and in increasing the effectiveness of vaccination.
Th1/Th2 Model for helper T cells edit
Proliferating helper T cells that develop into effector T cells differentiate into two major subtypes of cells known as Th1 and Th2 cells also known as Type 1 and Type 2 helper T cells, respectively.
Th1 helper cells are the host immunity effectors against intracellular bacteria and protozoa. They are triggered by IL-12, IL-2 and their effector cytokine is IFN-γ. The main effector cells of Th1 immunity are macrophages as well as CD8 T cells, IgG B cells, and IFN-γ CD4 T cells. The key Th1 transcription factors are STAT4 and T-bet. IFN-γ secreted by CD4 T cells can activate macrophages to phagocytose and digest intracellular bacteria and protozoa. In addition, IFN-γ can activate iNOS to produce NOx free radicals to directly kill intracellular bacteria and protozoa. Th1 overactivation against autoantigens will cause Type 4 delayed-type hypersensitivity. Tuberculin reaction or Type 1 diabetes belong to this category of autoimmunity. 1
Th2 helper cells are the host immunity effectors against extracellular parasites including helminths. They are triggered by IL-4 and their effector cytokines are IL-4, IL-5, IL-9, IL-10 and IL-13. The main effector cells are eosinophils, basophils, and mast cells as well as B cells, and IL-4/IL-5 CD4 T cells. The key Th2 transcription factors are STAT6 and GATAs. IL-4 is the positive feedback cytokine for Th2 cells differentiation. Besides, IL-4 stimulates B-cells to produce IgE antibodies, which in turn stimulate mast cells to release histamine, serotonin, and leukotriene to cause broncho-constriction, intestinal peristalsis, gastric fluid acidification to expel helminths. IL-5 from CD4 T cells will activate eosinophils to attack helminths. IL-10 suppresses Th1 cells differentiation and function of dendritic cells. Th2 overactivation against autoantigen will cause Type1 IgE-mediated allergy and hypersensitivity. Allergic rhinitis, atopic dermatitis, and asthma belong to this category of autoimmunity. 1 In addition to expressing different cytokines, Th2 cells also differ from Th1 cells in their cell surface glycans oligosaccharides, which makes them less susceptible to some inducers of cell death. 2 3
Th1/Th2 Model for helper T cells. An antigen is ingested and processed by an APC. It presents fragments from it to T cells. The upper, Th0, is a T helper cell. The fragment is presented to it by MHC2. 4 IFN-γ, interferon γ; TGF-β, transforming growth factor β; mø, macrophage; IL-2, interleukin 2; IL-4, interleukin 4
interferon-γ and TNF-β. Interleukin-2 interleukin-10 production has been reported in activated Th1 cell. 5
interleukin-4, interleukin-5, interleukin-6, interleukin-9, interleukin-10, interleukin-13
Cellular immune system. Maximizes the killing efficacy of the macrophages and the proliferation of cytotoxic CD8 T cells. Also promotes the production of IgG, an opsonizing antibody.
Humoral immune system. Stimulates B-cells into proliferation, to induce B-cell antibody class switching, and to increase neutralizing antibody production. IgG, IgM and IgA as well as IgE antibodies
The Type 1 cytokine IFN-γ increases the production of interleukin-12 by dendritic cells and macrophages, and via positive feedback, IL-12 stimulates the production of IFN-γ in helper T cells, thereby promoting the Th1 profile. IFN-gamma also inhibits the production of cytokines such as interleukin-4, an important cytokine associated with the Type 2 response, and thus it also acts to preserve its own response.
The Type 2 response promotes its own profile using two different cytokines. Interleukin-4 acts on helper T cells to promote the production of Th2 cytokines including itself; it is auto-regulatory, while interleukin-10 IL-10 inhibits a variety of cytokines including interleukin-2 and IFN-γ in helper T cells and IL-12 in dendritic cells and macrophages. The combined action of these two cytokines suggests that once the T cell has decided to produce these cytokines, that decision is preserved and also encourages other T cells to do the same.
While we know about the types of cytokine patterns helper T cells tend to produce, we understand less about how the patterns themselves are decided. Various evidence suggests that the type of APC presenting the antigen to the T cell has a major influence on its profile. Other evidence suggests that the concentration of antigen presented to the T cell during primary activation influences its choice. The presence of some cytokines such as the ones mentioned above will also influence the response that will eventually be generated, but our understanding is nowhere near complete.
Main article: T helper 17 cell
Th17 helper cells are a subset of T helper cells developmentally distinct from Th1 and Th2 lineages producing interleukin 17 IL-17.
THαβ helper cells provide the host immunity against viruses. Their differentiation is triggered by IFN alpha/beta or IL-10. Their key effector cytokine is IL-10. Their main effector cells are NK cells as well as CD8 T cells, IgG B cells, and IL-10 CD4 T cells. The key THαβ transcription factors are STAT1 and STAT3 as well as IRFs. IL-10 from CD4 T cells activate NK cells ADCC to apoptose virus-infected cells and to induce host as well as viral DNA fragmentation. IFN alpha/beta can suppress transcription to avoid virus replication and transmission. Overactivation of THαβ against autoantigen will cause type 2 antibody-dependent cytotoxic hypersensitivity. Myasthenia gravis or Graves disease belong to this category. 6
Limitations to the Th1/Th2 model edit
The interactions between cytokines from the Th1/Th2 model can be more complicated in some animals. For example, the Th2 cytokine IL-10 inhibits cytokine production of both Th subsets in humans. Human IL-10 hIL-10 suppresses the proliferation and cytokine production of all T cells and the activity of macrophages, but continues to stimulate plasma cells, ensuring that antibody production still occurs. As such, hIL-10 is not believed to truly promote the Th2 response in humans, but acts to prevent over-stimulation of helper T cells while still maximising the production of antibodies.
There are also other types of T cells that can influence the expression and activation of helper T cells, such as natural regulatory T cells, along with less common cytokine profiles such as the Th3 subset of helper T cells. Terms such as regulatory and suppression have become ambiguous after the discovery that helper CD4 T cells are also capable of regulating and suppressing their own responses outside of dedicated regulatory T cells.
One major difference between regulatory T cells and effector T cells is that regulatory T cells typically serve to modulate and deactivate the immune response, while effector T cell groups usually begin with immune-promoting cytokines and then switch to inhibitory cytokines later in their life cycle. The latter is a feature of Th3 cells, which transform into a regulatory subset after its initial activation and cytokine production.
Both regulatory T cells and Th3 cells produce the cytokine transforming growth factor-beta TGF-β and IL-10. Both cytokines are inhibitory to helper T cells; TGF-β suppresses the activity of most of the immune system. There is evidence to suggest that TGF-β may not suppress activated Th2 cells as effectively as it might suppress naive cells, but it is not typically considered a Th2 cytokine.
The characterisation of another novel T helper subtype, T helper 17 cells Th17 7 has cast further doubt on the basic Th1/Th2 model. These IL-17 producing cells were initially described as a pathogenic population implicated in autoimmunity but are now thought to have their own distinct effector and regulatory functions. Of note, recent evidence suggest that functional plasticity is an intrinsic capacity of T helper cells. Indeed, a study in mice demonstrated that Th17 cells transform into Th1 cells in vivo. 8 A subsequent study furthermore showed that extensive T helper cell plasticity is also prominent in man. 9
Many of the cytokines in this article are also expressed by other immune cells see individual cytokines for details, and it is becoming clear that while the original Th1/Th2 model is enlightening and gives insight into the functions of helper T cells, it is far too simple to define its entire role or actions. Some immunologists question the model completely, as some in vivo studies suggest that individual helper T cells usually do not match the specific cytokine profiles of the Th model, and many cells express cytokines from both profiles. 10 That said, the Th model has still played an important part in developing our understanding of the roles and behaviour of helper T cells and the cytokines they produce during an immune response.
Recent scientific studies by Stockinger et al. revealed that another T helper subset may exist. Th9 cells are claimed to be an IL9 interleukin 9 –producing T cell subset focused on defending helminth infections. 11
Role of helper T cells in disease edit
Considering the diverse and important role helper T cells play in the immune system, it is not surprising that these cells often influence the immune response against disease. They also appear to make occasional mistakes, or generate responses that would be politely considered non-beneficial. In the worst-case scenario, the helper T cell response could lead to a disaster and the fatality of the host. Fortunately this is a very rare occurrence.
Main article: CD4 T cells and antitumor immunity
Helper T cells and hypersensitivity edit
The immune system must achieve a balance of sensitivity in order to respond to foreign antigens without responding to the antigens of the host itself. When the immune system responds to very low levels of antigen that it usually shouldn t respond to, a hypersensitivity response occurs. Hypersensitivity is believed to be the cause of allergy and some auto-immune disease.
Hypersensitivity reactions can be divided into four types:
Type 1 hypersensitivity includes common immune disorders such as asthma, allergic rhinitis hay fever, eczema, urticaria hives and anaphylaxis. These reactions all involve IgE antibodies, which require a Th2 response during helper T cell development. Preventive treatments, such as corticosteroids and montelukast, focus on suppressing mast cells or other allergic cells; T cells do not play a primary role during the actual inflammatory response. It s important to note that the numeral allocation of hypersensitivity types does not correlate and is completely unrelated to the response in the Th model.
Type 2 and Type 3 hypersensitivity both involve complications from auto-immune or low affinity antibodies. In both of these reactions, T cells may play an accomplice role in generating these auto-specific antibodies, although some of these reactions under Type 2 hypersensitivity would be considered normal in a healthy immune system for example, Rhesus factor reactions during child-birth is a normal immune response against child antigens. The understanding of the role of helper T cells in these responses is limited but it is generally thought that Th2 cytokines would promote such disorders. For example, studies have suggested that lupus SLE and other auto-immune diseases of similar nature can be linked to the production of Th2 cytokines.
Type 4 hypersensitivity, also known as delayed type hypersensitivity, are caused via the over-stimulation of immune cells, commonly lymphocytes and macrophages, resulting in chronic inflammation and cytokine release. Antibodies do not play a direct role in this allergy type. T cells play an important role in this hypersensitivity, as they activate against the stimulus itself and promote the activation of other cells; particularly macrophages via Th1 cytokines.
Other cellular hypersensitivities include cytotoxic T cell mediated auto-immune disease, and a similar phenomenon; transplant rejection. Helper T cells are required to fuel the development of these diseases. In order to create sufficient auto-reactive killer T cells, interleukin-2 must be produced, and this is supplied by CD4 T cells. CD4 T cells can also stimulate cells such as natural killer cells and macrophages via cytokines such as interferon-gamma, encouraging these cytotoxic cells to kill host cells in certain circumstances.
The mechanism that killer T cells use during auto-immunity is almost identical to their response against viruses, and some viruses have been accused of causing auto-immune diseases such as Type 1 Diabetes mellitus. Cellular auto-immune disease occurs because the host antigen recognition systems fail, and the immune system believes, by mistake, that a host antigen is foreign. As a result, the CD8 T cells treat the host cell presenting that antigen as infected, and go on to destroy all host cells or in the case of transplant rejection, transplant organ that express that antigen.
Some of this section is a simplification. Many auto-immune diseases are more complex. A well-known example is rheumatoid arthritis, where both antibodies and immune cells are known to play a role in the pathology. Generally the immunology of most auto-immune diseases is not well understood.
Perhaps the best example of the importance of CD4 T cells is demonstrated with human immunodeficiency virus HIV infection. HIV mainly targets lymphoid CD4 T cells, but can infect other cells that express CD4 such as macrophages and dendritic cells both groups express CD4 at low levels.
It has been proposed that during the non-symptomatic phase of HIV infection, the virus has a relatively low affinity towards T cells and has a higher affinity for macrophages, resulting in a slow kill rate of CD4 T cells by the immune system citation needed. This is initially compensated for via the production of new helper T cells from the thymus originally from the bone marrow. Once the virus becomes lymphotropic or T-tropic however, it begins to infect CD4 T cells far more efficiently likely due to a change in the co-receptors it binds to during infection, and the immune system is overwhelmed. Of note, recent studies suggest that only 5 of the lymphoid-derived CD4 T cells targeted by HIV are permissive and become productively infected with the virus. More than 95 of the CD4 T cells that die are resting and are unable to support productive infection. These cells undergo abortive infection with HIV. 12 Cell death is triggered when the host cell detects HIV foreign DNA intermediates and initiates a suicidal death pathway in an attempt to protect the host, leading to caspase-1 activation in inflammasome and pyroptosis, a highly inflammatory form of programmed cell death. 13 14
At this point chronic inflammation ensues, and functional CD4 T cell levels begin to decrease, eventually to a point where the CD4 T cell population is too small to recognize the full range of antigens that could potentially be detected. The depletion of CD4 T cells and the development of chronic inflammation are signature processes in HIV pathogenesis that propel progression to acquired immune deficiency syndrome AIDS. CD4 T cell depleted to the cell count of less than 200cell/μL in blood during AIDS allows various pathogens to escape T cell recognition, thus allowing opportunistic infections that would normally elicit a helper T cell response to bypass the immune system. 15 While these complete bypass situations only occur when the helper T cell response is absolutely necessary for infection clearance, most infections increase in severity and/or duration because the immune system s helper T cells provide less efficient immune response.
Two components of the immune system are particularly affected in AIDS, due to its CD4 T cell dependency:
CD8 T cells are not stimulated as effectively during the AIDS stage of HIV infection, making AIDS patients very susceptible to most viruses, including HIV itself. This decline in killing of CD4 T cells results in the virus being produced for a longer period the infected CD4 T cells are not killed as quickly, increasing the proliferation of the virus, and accelerating the development of the disease.
Antibody class switching declines significantly once helper T cell function fails. The immune system loses its ability to improve the affinity of their antibodies, and are unable to generate B cells that can produce antibody groups such as IgG and IgA. These effects are primarily due to the loss of any helper T cell that can interact with the B lymphocyte correctly. Another symptom of AIDS is the reduction in antibody levels due to a decrease in Th2 cytokines and less interactions by helper T cells. All of these complications result in an increased susceptibility to aggressive bacterial infections, especially in areas of the body not accessible by IgM antibodies.
If the patient does not respond to or does not receive HIV treatment they will succumb usually to either cancers or infections; the immune system finally reaches a point where it is no longer coordinated or stimulated enough to deal with the disease.
Inhibition of CD4 T-cell expansion during HIV infection may occur due to microbial translocation in an IL-10-dependent way. Triggering PD-1 expressed on activated monocytes by its ligand PD-L1, induces IL-10 production which inhibits CD4 T-cell function. 16
CD4 T cells and antitumor immunity
a b c Zhu, J.; Paul, W. E. 2008. CD4 T cells: Fates, functions, and faults. Blood 112 5 : 1557. doi:10.1182/blood-2008-05-078154. PMID 18725574.
Maverakis E, Kim K, Shimoda M, Gershwin M, Patel F, Wilken R, Raychaudhuri S, Ruhaak LR, Lebrilla CB 2015. Glycans in the immune system and The Altered Glycan Theory of Autoimmunity. J Autoimmun 57 6 : 1–13. doi:10.1016/j.jaut.2014.12.002. PMID 25578468.
Toscano MA, Bianco GA, Ilarregui JM, Croci DO, Correale J, Hernandez JD, Zwirner NW, Poirier F, Riley EM, Baum LG, Rabinovich GA. 2007. Differential glycosylation of TH1, TH2 and TH-17 effector cells selectively regulates susceptibility to cell death. Nat Immunol 8 : 825–34.
Rang, H. P. 2003. Pharmacology. Edinburgh: Churchill Livingstone. ISBN 0-443-07145-4. Page 223
Saraiva M., Christensen J.R., Veldhoen M., Murphy T.L., Murphy K.M., O Garra A. 2009. Interleukin-10 production by Th1 cells requires interleukin-12-induced STAT4 transcription factor and ERK MAP kinase activation by high antigen dose. Immunity 31 2 : 209–219. doi:10.1016/j.immuni.2009.05.012. PMID 19646904.
Hu, Wanchung 2007. Microarray analysis of PBMC gene expression profiles after Plasmodium falciparum malarial infection Ph.D. thesis. Johns Hopkins University.
Harrington, LE; Hatton, RD; Mangan, PR; Turner, Henrietta; Murphy, Theresa L; Murphy, Kenneth M; Weaver, Casey T 2005. Interleukin 17-producing CD4 effector T cells develop via a lineage distinct from the T helper type 1 and 2 lineages. Nature Immunology 6 11 : 1023–32. doi:10.1038/ni1254. PMID 16200070
Hirota K, Duarte JH, Veldhoen M, Hornsby E, Li Y, Cua DJ, Ahlfors H, Wilhelm C, Tolaini M, Menzel U, Garefalaki A, Potocnik AJ, Stockinger B. Nat Immunol; Duarte; Veldhoen; Hornsby; Li; Cua; Ahlfors; Wilhelm; Tolaini; Menzel; Garefalaki; Potocnik; Stockinger 2011. Fate mapping of IL-17-producing T cells in inflammatory responses. Nature Immunology 12 3 : 255–63. doi:10.1038/ni.1993. PMC 3040235. PMID 21278737.
Larsen M, Arnaud L, Hie M, Parizot C, Dorgham K, Shoukry M, Kemula M, Barete S, Derai D, Sauce D, Amoura Z, Pene J, Yssel H, Gorochov G. Eur J Immunol; Arnaud; Hié; Parizot; Dorgham; Shoukry; Kemula; Barete; Derai; Sauce; Amoura; Pène; Yssel; Gorochov 2011. Multiparameter grouping delineates heterogeneous populations of human IL-17 and/or IL-22 T-cell producers that share antigen specificities with other T-cell subsets. European Journal of Immunology UPMC Paris 06 Institut National de la Santé et de la Recherche Médicale Inserm UMR-S 945 41 9 : 2596–2605. doi:10.1002/eji.201041131. PMID 21688259.
Nakayamada S., Takahashi H., Kanno Y., O Shea J.J. 2012. Helper T cell diversity and plasticity. Current Opinion in Immunology 24 3 : 297–302. doi:10.1016/j.coi.2012.01.014. PMID 22341735.
Veldhoen and Stockinger, Dardalhon and Kuchroo both papers from Nature Immunology 2008
Doitsh G. et al Cell 2010 Abortive HIV Infection Mediates CD4 T Cell Depletion and Inflammation in Human Lymphoid Tissue
Doitsh G. et al Nature 2013 Cell death by pyroptosis drives CD4 T-cell depletion in HIV-1 infection
Monroe KM et al Science 2013 IFI16 DNA Sensor Is Required for Death of Lymphoid CD4 T Cells Abortively Infected with HIV
CD4 Count. www.aids.gov. Retrieved 2015-04-30.
Said E.A., Dupuy F.P., Trautmann L., Zhang Y., Shi Y., El-Far M., Hill B.J., Noto A., Ancuta P., Peretz Y., Fonseca S.G., Van Grevenynghe J., Boulassel M.R., Bruneau J., Shoukry N.H., Routy J.P., Douek D.C., Haddad E.K., Sekaly R.P. 2010. Programmed death-1-induced interleukin-10 production by monocytes impairs CD4 T cell activation during HIV infection. Natural Medicine 16 4 : 452–459. doi:10.1038/nm.2106. PMID 20208540.
Kanno Y, Vahedi G, Hirahara K, Singleton K and O Shea JJ. 2012. Transcriptional and Epigenetic Control of T Helper Cell Specification: Molecular Mechanisms Underlying Commitment and Plasticity. Annual Review of Immunology 30: 707-731.
In SLE patients, T helper type 1 polarisation is more abundant rather than type 2, where the main cytokine profile are Inf gama from T cells and its consequence interferon alpha high range production by DC.
T-cell Group - Cardiff University
Retrieved from https://en.wikipedia.org/w/index.php.title T_helper_cell oldid 691236279
Categories: T cellsHuman cells.
9-2. Armed helper T cells activate B cells that recognize the same antigen. T-cell dependent antibody responses require the activation of B cells by helper T cells.